Despite the growing evidence of the effects of social determinants of health (SDOH) on both short- and long-term health outcomes, there is little emphasis on developing theory- and evidence-based multilevel and population (community) interventions that target both structural and individual factors. For these interventions to be effective, it necessitates the development of new measures; the adaptation of existing measures of SDOH; and a comprehensive understanding of the pathways by which the social context affects health.
While focusing on improving the health of the population, it is imperative to ensure that every sector of society benefits equally from the developments in health. In this regard, research in small populations that are largely excluded from clinical trials and interventions due to the limited size of these populations, need to be encouraged with appropriate methodologies and measures.
- How can models comparing the effects of social context on health patterns and trends within various settings – including community and clinical settings – be developed? What are the common measures? How can we develop measures which are interoperable?
- How would real-time data and the changing technology be garnered to have greater impact on health promotion and disease prevention in low- income and “hard-to-reach” populations. (e.g., those in rural and remote areas)?
- How does social context contribute to differences in cancer incidence and mortality?
- How can interventions be developed and implemented that measure and include the social context and address the social needs of the population?
- How can increased knowledge of the global cancer burden contribute to our understanding of cancer outcomes in the United States?
- What are the key factors (including psychological, social, environmental, and policy-level) influencing cancer prevention strategies? How can these multilevel interventions be sustainable in real-life context?
- How can culturally appropriate interventions among indigent populations (including cancer survivors) be designed and implemented to improve the health and quality of life?
- To what extent are clinical and community-based intervention programs designed to address differences in cancer outcomes informed by evidence from science, practice, and policy?
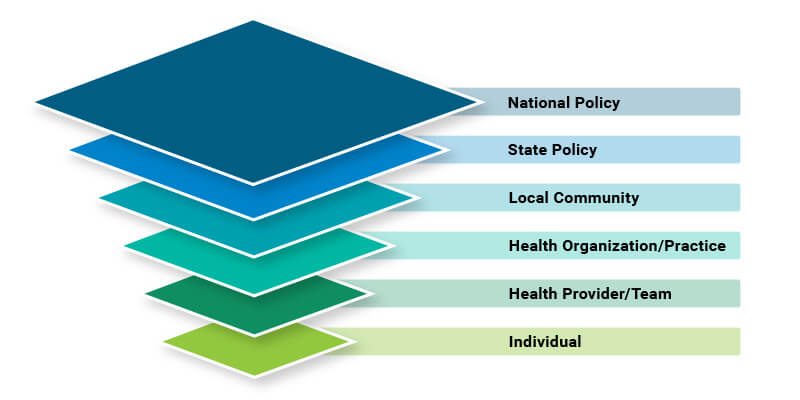
Multilevel Influences on Cancer Control
- What statistical tools are needed to analyze this kind of data?
- Can evidence-based interventions from other large populations be adapted to smaller populations? What are the factors that need to be considered when testing and implementing multilevel interventions? Is there sufficient statistical power to assess the effects of each level and tease them apart?
- Given the diverse locations of the subpopulations, how can concept of place be incorporated in these studies? Can these differences in communities be explained by the social, environmental, or ecological factors? How can these factors be measured and included in interventions?

