Background
Cancer survivorship care is complex and multifaceted. The landmark Lost in Transition report from the Institute of Medicine (IOM), now the National Academy of Medicine, recommended comprehensive care after a cancer diagnosis, including prevention and surveillance for recurrence and new cancers, surveillance and management of physical and psychosocial effects of cancer and its treatment, and health promotion/preventive care. These components of care necessitate coordination, often among multiple providers.
The phrase models of survivorship care refers to the type of care being delivered and which providers are delivering the care, when, and to whom. There are many models of survivorship care, including (but not limited to) oncology-led, primary care-led, shared care, and multidisciplinary survivorship clinics.
Oncology-led care involves survivors receiving their survivorship care primarily from an oncology provider. Primary care-led survivorship care places the primary care provider (PCP) as the lead to coordinate the components of survivorship care. However, many professional organizations have advocated for survivorship care that involves multiple providers. One example of this is the multidisciplinary survivorship clinic, where survivors receive different types of care from multiple providers in a separate clinical area, often within the same visit. Another example is shared survivorship care, which has been identified by many as the optimal model of care. Shared care is a collaborative approach that has enhanced communication and coordination among oncology providers, PCPs, and other specialists as needed. The model of care that survivors receive may depend on many factors, including survivor needs, provider preference, and healthcare system resources.
While there are many models of survivorship care, there is growing recognition that one model is not right for all cancer survivors. Many survivorship clinicians, researchers, and professional organizations have advocated for risk-stratified survivorship care1,2,3. Risk-stratified survivorship care describes a personalized approach in which cancer survivors are triaged, or stratified, to distinct care pathways based on the complexity of their needs and the types of providers their care requires.
The National Cancer Institute (NCI) Office of Cancer Survivorship (OCS) and the Division of Cancer Control and Population Sciences has supported several initiatives focused on improving care for cancer survivors by studying models of care, which includes risk-stratified care. This work is expected to improve our understanding of the care needs of survivors and identify and evaluate strategies to improve care delivery and outcomes.
Described below are activities, funding opportunities, and resources in this important area of research.
Developing a Quality of Cancer Survivorship Care Framework
One of the key recommendations in the IOM Lost in Transition report stated that “quality of survivorship care measures should be developed…to monitor and improve the care that all survivors receive.” In attempts to fulfill this recommendation, several initiatives have been launched, including the American College of Surgeons Commission on Cancer standards for survivorship care that were required for cancer program accreditation, and the American Society of Clinical Oncology Quality Oncology Practice Initiative, among others. Although these efforts are likely to improve care for cancer survivors, their scope has been limited with respect to addressing the breadth of cancer survivorship care.
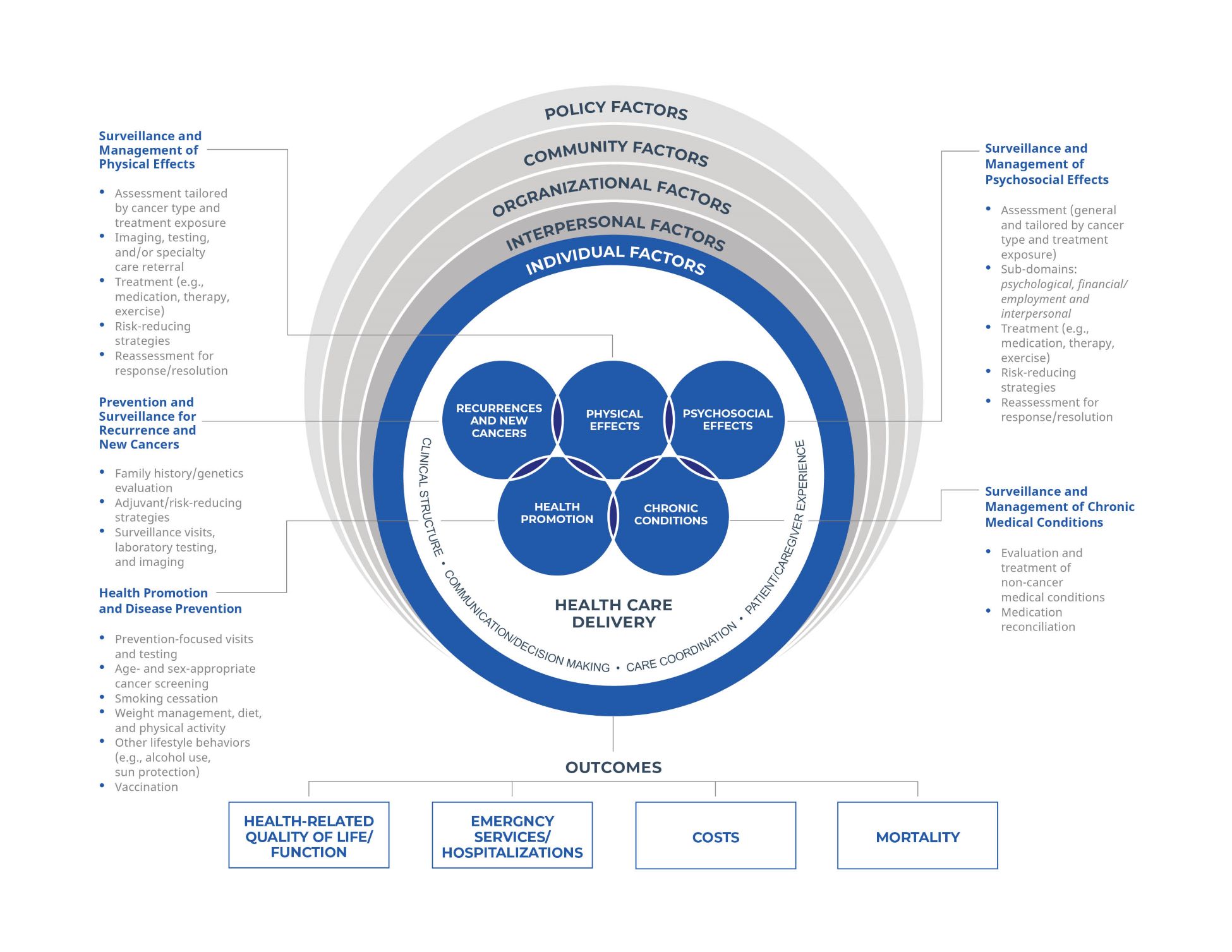
In response to this scientific gap, Dr. Larissa Nekhlyudov from Brigham and Women’s Hospital, Harvard Medical School, in collaboration with NCI experts, developed a comprehensive, evidence-based quality of cancer survivorship care framework. This involved an extensive review of several sources to identify key domains in survivorship care quality, including cancer survivor and site-specific guidelines, the NIH grant portfolio, US cancer control plans, quality measures, and survivor forums. The team then conducted semi-structured interviews with key experts to refine the framework and convened a meeting to discuss the framework and its implications.
The framework below is intended to serve as the foundation to define the key components of survivorship care and to inform the identification and development of quality metrics to measure and improve care for survivors.
Risk-stratified Survivorship Care
Although risk-stratified survivorship care has been implemented for survivors of some cancers internationally,4,5 this approach to survivorship care has been largely untested in the US. Overall, there is a lack of evidence-based algorithms to risk stratify survivors for most types of cancer, and even among those cancer types where risk-stratified algorithms exist, there has been limited research evaluating outcomes of risk-stratified care pathways.
Thus, the questions that survivors, clinicians, and policymakers need answers to are (1) What factors/variables should be considered in a risk-stratified survivorship care pathway algorithm?; and (2) What is the effectiveness of implementing an existing risk-stratified survivorship care model on quality of care, survivor outcomes, and health care utilization?
To address these questions, NCI published two funding opportunities to advance research on risk-stratified survivorship care.
Notice of Special Interest (NOSI): Administrative Supplements for Development of Risk-Stratified Cancer Survivorship Care Algorithms
NOT-CA-20-038 was published in 2020 to indicate NCI’s interest in supplement applications that propose methodological approaches to identify individuals within low-, medium-, and high-need groups in a risk-stratified survivorship care algorithm. This work was intended to inform future development of risk-stratified care pathways based on developed algorithms. Through this supplement, seven awards were funded, and several used existing data from NCI-funded cohorts and intervention studies, in combination with additional sources (e.g., electronic health records) to develop risk-stratified algorithms for multiple cancer types. Applications focused on several aspects of comprehensive survivorship care, including care for chronic health conditions, symptom management, cardiovascular risk, and screening for recurrence and subsequent cancers. This foundational work will allow for future algorithm validation and development of tailored survivorship care pathways.
Notice of Special Interest (NOSI): Tailoring Follow-up Care for Survivors Using Risk-Stratified Pathways
NOT-CA-21-019 was published to highlight NCI’s interest in receiving applications focused on identifying important factors for defining risk-stratified survivorship care or developing and testing approaches to improve the clinical management and outcomes for adult cancer survivors using risk-stratified survivorship care pathways.
Though these funding opportunities are no longer active, OCS is committed to advancing the science of risk-stratified survivorship care. Please contact Dr. Lisa Gallicchio or Dr. Michelle Mollica to discuss your grant application ideas.
Pediatric, Adolescent, and Young Adult Cancer Survivorship Care
Improving care delivery for survivors of pediatric, adolescent, and young adult cancers was a key priority in the Childhood Cancer Survivorship, Treatment, Access, and Research (STAR) Act. NCI has supported several funding opportunities and initiatives that include aims to improve models of care for these survivors, such as a trans-NIH initiative focused on transitions between pediatric and adult health care for children with serious illnesses, including cancer. You can read more about NCI’s efforts here.
Telehealth
There has been a substantial increase in telehealth use in the United States. Research has shown that telehealth can improve health care access and quality, patient-provider communication, and health outcomes. Many aspects of cancer care can be delivered through telehealth, such as promotion of positive health behaviors and cancer screening, remote patient monitoring and management of symptoms during cancer treatment, as well as survivorship follow-up care.
NCI’s Telehealth Research Centers of Excellence (TRACE) initiative funds multiple centers focused on the integration of telehealth across the cancer continuum, including survivorship. More information on the TRACE centers can be found here.
Additional discussion about the surge in telehealth-based cancer care during the COVID-19 pandemic can be found in this NCI Cancer Currents blog. And this NCI Cancer Currents blog focuses on a 2023 study that found that telehealth can save people with cancer time, travel, and money.
Additional Related Funding Opportunity Announcements (also called Notices of Funding Opportunities, or NOFOs)
RFA-CA-19-035: Optimizing the Management and Outcomes for Cancer Survivors Transitioning to Follow-up Care
The purpose of this RFA was to fund grants that focused on the development and testing of innovative, feasible, and effective models of care for adult survivors of cancer who are transitioning from active treatment to follow-up care. Specifically, grants proposed a multilevel intervention aimed at enhancing communication, collaboration, and coordination among oncology and non-oncology providers to improve survivor outcomes. This RFA, supported through the Cancer Moonshot, funded five awards focused on a breadth of cancer survivor populations and components of care.
RFA-CA-23-025: Addressing the Needs of Cancer Survivors in Primary Care (U01 Clinical Trial Required)
The purpose of this RFA was to support studies that aim to develop and test primary care practice-level and health system-level interventions and strategies that promote high quality care for cancer survivors during and/or after the treatment period. This research will inform the critically needed evidence base for delivery of high-quality survivorship care provided in part by PCPs. You can learn more about NCI’s efforts to advance research on primary care and cancer survivorship here.
Events
The OCS Director’s Series has featured webinars focused on models of survivorship care.
Dr. Simon Craddock Lee - Optimizing Care Delivery for Cancer Survivors: Engaged, Pragmatic, Multi-team & Multi-level (September 2023)
Dr. Ray Chan – Innovations in Survivorship Models of Care (February 2023)
Dr. Shawna Hudson – Cancer Survivorship Healthcare Delivery: Challenges and Opportunities Integrating Primary Care (September 2021)
Additional Resources
- Hewitt M, Greefield S, Stovall E, eds. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, D.C.: The National Academies Press; 2006. https://nap.nationalacademies.org/catalog/11468/from-cancer-patient-to-cancer-survivor-lost-in-transition

- The Oncology Nursing Podcast. Which Survivorship Care Model Is Right for Your Patient? with Michelle Mollica, PhD, MPH, RN, OCN. April 2022. Accessed May 24, 2023. https://onsvoice.libsyn.com/website/episode-201-which-survivorship-care-model-is-right-for-your-patient
 .
. - Nekhlyudov L, Mollica MA, Jacobsen PB, Mayer DK, Shulman LN, Geiger AM. Developing a quality of cancer survivorship care framework: implications for clinical care, research, and policy. J Natl Cancer Inst. 2019;111(11):1120-1130. doi:10.1093/jnci/djz089.
- Tonorezos ES, Barnea D, Cohn RJ, et al. Models of care for survivors of childhood cancer from across the globe: advancing survivorship care in the next decade. J Clin Oncol. 2018;36(21):2223-2230. doi:10.1200/JCO.2017.76.5180.
- Mollica M, Mayer DK, Oeffinger KE, et al. Follow up care for breast and colorectal cancer across the globe: survey findings from 27 countries. JCO Glob Oncol. 2020;6:1394-1411. doi:10.1200/GO.20.00180
 .
. - Mayer D, Alfano C. Personalized risk-stratified cancer follow-up care: its potential for healthier survivors, happier clinicians, and lower costs. J Natl Cancer Inst. 2019;111(5):442-448. doi:10.1093/jnci/djy232.
- Alfano C, Jefford M, Maher J, Birken SA, Mayer DK. Building personalized cancer follow-up care pathways in the United States: lessons learned from implementation in England, Northern Ireland, and Australia. ASCO Educational Book. https://ascopubs.org/doi/full/10.1200/EDBK_238267
 . Accessed May 24, 2023.
. Accessed May 24, 2023. - Alfano C, Mayer DK, Bhatia S, et al. Implementing personalized pathways for cancer follow-up care in the United States: proceedings from an American Cancer Society–American Society of Clinical Oncology summit. CA Cancer J Clin. 2019;69(3):234-247. doi:10.3322/caac.21558
 .
.
Footnotes
1Mayer D, Alfano C. Personalized risk-stratified cancer follow-up care: its potential for healthier survivors, happier clinicians, and lower costs. J Natl Cancer Inst. 2019;111(5):442-448. doi:10.1093/jnci/djy232 ![]() .
.
2Alfano C, Jefford M, Maher J, Birken SA, Mayer DK. Building personalized cancer follow-up care pathways in the United States: lessons learned from implementation in England, Northern Ireland, and Australia. ASCO Educational Book. https://ascopubs.org/doi/full/10.1200/EDBK_238267 ![]() . Accessed May 24, 2023.
. Accessed May 24, 2023.
3Alfano C, Mayer DK, Bhatia S, et al. Implementing personalized pathways for cancer follow-up care in the United States: proceedings from an American Cancer Society–American Society of Clinical Oncology summit. CA Cancer J Clin. 2019;69(3):234-247. doi:10.3322/caac.21558 ![]() .
.
4Mollica M, Mayer DK, Oeffinger KE, et al. Follow up care for breast and colorectal cancer across the globe: survey findings from 27 countries. JCO Glob Oncol. 2020;6:1394-1411. doi:10.1200/GO.20.00180 ![]() .
.
5Mayer D, Alfano C. Personalized risk-stratified cancer follow-up care: its potential for healthier survivors, happier clinicians, and lower costs. J Natl Cancer Inst. 2019;111(5):442-448. doi:10.1093/jnci/djy232 ![]() .
.