Advancing health equity in cancer survivorship is central to the Office of Cancer Survivorship (OCS) mission to enhance the quality and length of survival of all persons diagnosed with cancer.
All cancer survivors should have the opportunity to achieve their highest level of health possible, also known as health equity. Unfortunately, there are obstacles to health related to where cancer survivors live, grow, learn, work, play, worship, access care, and age. These barriers can create differences in healthcare utilization, quality of care, and health outcomes, also known as health disparities.
How is NCI Addressing Issues Related to Health Disparities?
The causes the these health differences are multiple, multilevel, complex, and intertwined. However, researchers, advocacy groups, community organizations, health systems, clinicians, cancer survivors, caregivers, and other collaborators can work together to identify and intervene upon the modifiable obstacles, pathways, and mechanisms that create and amplify health disparities.
Selected examples of health equity research in cancer survivorship include the following:
- evaluating the available resources, opportunities, and built environment to help cancer survivors engage in and sustain healthy behaviors
- advancing access to survivorship care by testing new models of care, implementing the newly developed National Standards for Cancer Survivorship Care, and examining the roles of expanded health coverage and access to specialized cancer centers and survivorship services
- exposing how poverty contributes to conditions that lead to financial hardship
Areas of Research Emphasis
OCS, along with other divisions, programs, and offices of NCI and NIH, supports innovative research to enhance the quality and length of survival of all persons diagnosed with cancer. A recent analysis of the NIH Cancer Survivorship Portfolio from Fiscal Years 2017 to 2022 identified 147 grants focused on NIH-designated populations that experience health disparities.
Inclusion
Seventy-four percent of those identified NIH grants were focused on cancer survivors from underrepresented populations. There was a lack of grants focused on cancer survivors from American Indian and Alaska Native populations, Native Hawaiian and other Pacific Islander populations, and sexual and gender minority populations.
Note: Grants may focus on more than one of these populations. Therefore, the sum of the percentages is more than 100.
Data source: Doose M, Mollica MA, Acevedo AM, Tesauro G, Gallicchio L, Reed C, Guida J, Maher ME, Srinivasan S, Tonorezos E. Advancing health equity in cancer survivorship research: National Institutes of Health 2017-2022 portfolio review. J Natl Cancer Inst. 2024 Mar 27:djae073. doi: 10.1093/jnci/djae073. Epub ahead of print. PMID: 38544292.
Measures
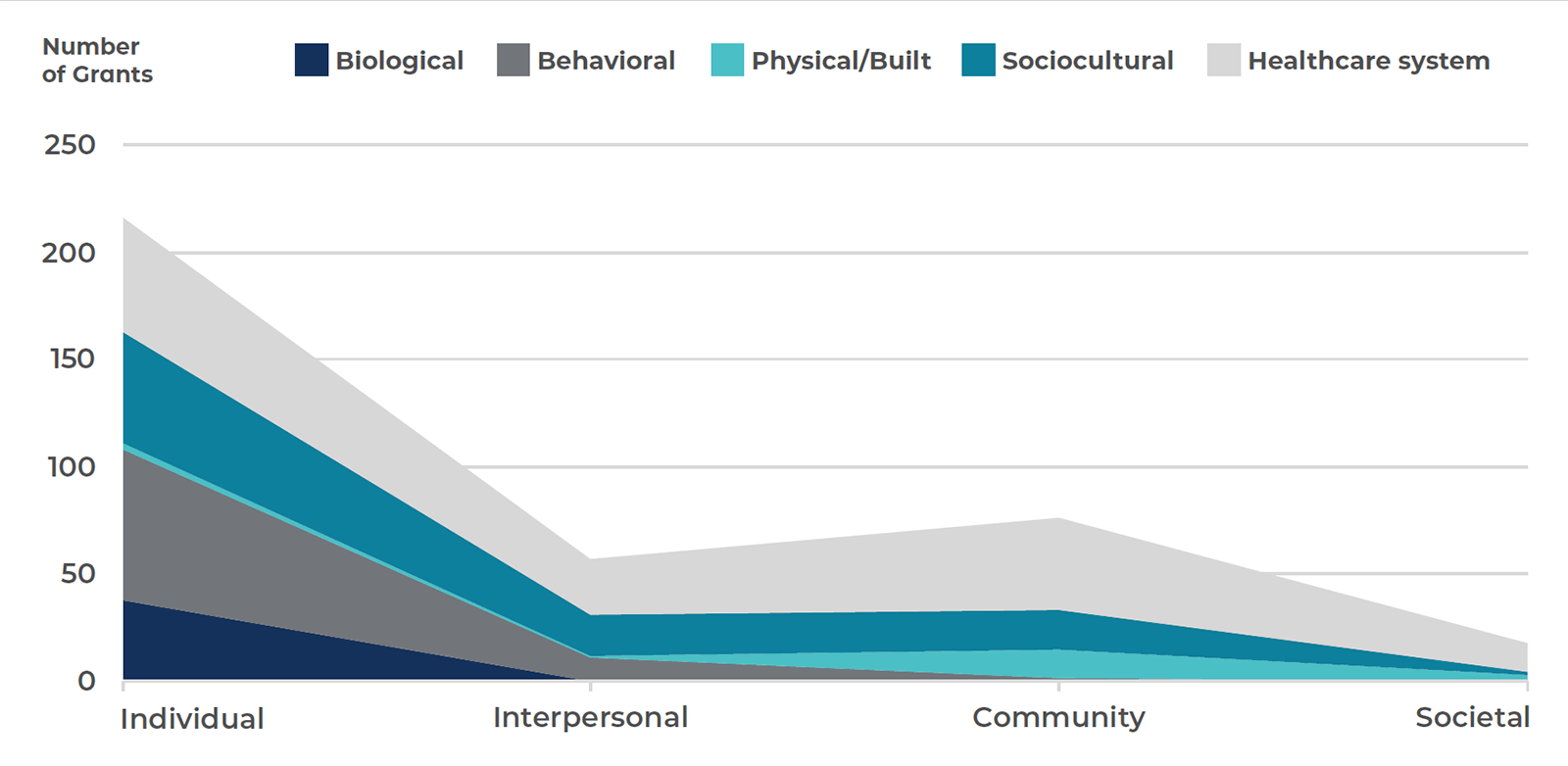
The majority of identified NIH grants measured or intervened at the individual level (82%), such as cancer survivors’ behaviors and healthcare use. The societal level and physical and built environment were least addressed (see figure below).
Other levels included:
- interpersonal level (e.g., relationships between cancer survivor and caregiver, or social networks); 33%
- community level (e.g., hospitals or neighborhoods); 42%
- societal level (e.g., states or countries); 12%
Note: This graph shows the distribution of grants that measured or intervened upon health disparities at each domain and level of influence. Each grant could measure at multiple domains and levels, and therefore the total exceeds 147 grants.
Data source: Doose M, Mollica MA, Acevedo AM, Tesauro G, Gallicchio L, Reed C, Guida J, Maher ME, Srinivasan S, Tonorezos E. Advancing health equity in cancer survivorship research: National Institutes of Health 2017-2022 portfolio review. J Natl Cancer Inst. 2024 Mar 27:djae073. doi: 10.1093/jnci/djae073. Epub ahead of print. PMID: 38544292.
The figure below highlights selected grant topics from the NIH Cancer Survivorship Portfolio from Fiscal Years 2017 to 2022. Italicized text represents areas of research currently not in the portfolio. Opportunities to understand and address health disparities beyond the individual level of influence include policies and laws that affect behaviors at the societal level (e.g., alcohol or tobacco policies) and the physical and built environment within communities (e.g., housing, green space).
| LEVELS OF INFLUENCE | |||||
|---|---|---|---|---|---|
| Individual | Interpersonal | Institutional/community | Societal | ||
|
DOMAINS OF INFLUENCE |
Biological |
|
|
|
|
|
Behavioral |
|
|
|
|
|
|
Physical/built environment |
|
|
|
|
|
|
Sociocultural environment |
|
|
|
|
|
|
Healthcare system |
|
|
|
|
|
Doose M, Mollica MA, Acevedo AM, Tesauro G, Gallicchio L, Reed C, Guida J, Maher ME, Srinivasan S, Tonorezos E. Advancing health equity in cancer survivorship research: National Institutes of Health 2017-2022 portfolio review. J Natl Cancer Inst. 2024 Mar 27:djae073. doi: 10.1093/jnci/djae073. Epub ahead of print. PMID: 38544292.
Selected OCS Staff Publications
Included below is a selection of recent OCS staff publications related to health disparities and health equity research in cancer survivorship.
- Doose M, Kennedy AE, Williams SD, Srinivasan S. The Context of Poverty and Cancer: Denying Human Potential. Cancer Epidemiol Biomarkers Prev. 2024 Nov 1;33(11):1402-1404. doi: 10.1158/1055-9965.EPI-24-0953. PMID: 39482971
- Brick R, Tonorezos ES. Addressing Disability in Cancer Survivors. J Clin Oncol. 2024 May 9:JCO2400479. doi: 10.1200/JCO.24.00479. PMID: 38723210
- Doose M, Mollica MA, Acevedo AM, Tesauro G, Gallicchio L, Reed C, Guida J, Maher ME, Srinivasan S, Tonorezos E. Advancing health equity in cancer survivorship research: National institutes of health 2017-2022 portfolio review. J Natl Cancer Inst. 2024 Mar 27:djae073. doi: 10.1093/jnci/djae073. Epub ahead of print. PMID: 38544292.
- Verhoeven D, Doose M, Chollette V, Weaver SJ. Team complexity and care coordination for cancer survivors with multiple chronic conditions: a mixed methods study. J Cancer Surviv. 2024 Feb 14. doi: 10.1007/s11764-023-01488-w. Epub ahead of print. PMID: 38353854.
- Mollica MA, Zaleta AK, Gallicchio L, Brick R, Jacobsen PB, Tonorezos E, Castro KM, Miller MF. Financial toxicity among people with metastatic cancer: findings from the Cancer Experience Registry. Support Care Cancer. 2024 Jan 30;32(2):137. doi: 10.1007/s00520-024-08328-2. PMID: 38286846.
- Tonorezos E (editor). Journal of Cancer Survivorship Special Section: Hearing Loss in Cancer Survivorship. https://link.springer.com/collections/acfafeaiai
Selected Funding Opportunities
A list of funding opportunities related to health disparities and health equity in cancer survivorship research at NIH can be found on this Apply for Cancer Control Grants page.
Featured Webinars
The NCI OCS events webpage has archived webinars related to health equity and health disparities research in cancer survivorship. Here is a selected list of webinars.
Health Equity Research in Cancer Survivorship
- December 17, 2024—Mind Your BEAT: A Community-based Physical Activity Intervention for Rural Cancer Survivors (Dr. Mama)
- September 17, 2024—Implementing Patient-Reported Outcomes and Psychosocial Interventions in Diverse Communities of Cancer Survivors (Dr. Penedo)
- March 5, 2024—Partnership: A Mission and an Imperative for Health Equity-Focused Survivorship Research and Engagement
- October 17, 2023—Understanding and Addressing Housing Instability for Cancer Survivors
- September 19, 2023—Optimizing Care Delivery for Cancer Survivors: Engaged, Pragmatic, Multi-team & Multi-level
Focus on American Indians and Alaska Natives
- November 7, 2023—Beyond Survivance: Thrivance Among American Indian and Alaska Native Cancer Survivors
Focus on People with Disabilities
- January 24, 2023—Hear Today and Tomorrow: Unmet Needs and Opportunities for Improving Hearing Health in Cancer Survivors
- April 25, 2023—Improving Care for Cancer Survivors with Serious Mental Illness
Focus on Sexual and Gender Minority Groups
- January 31, 2023—The Rainbow Connection: Building a Career as an LGBTQ+ Scientist
- February 15, 2022—Disparities Among Sexual and Gender Minority Cancer Survivors: Studies on Prostate Cancer in Gay and Bisexual Men
Focus on Socioeconomic Status
Contacts

Michelle Doose, PhD, MPH
OFFICE OF CANCER SURVIVORSHIP
HEALTH COMMUNICATION AND INFORMATICS RESEARCH BRANCH
BEHAVIORAL RESEARCH PROGRAM