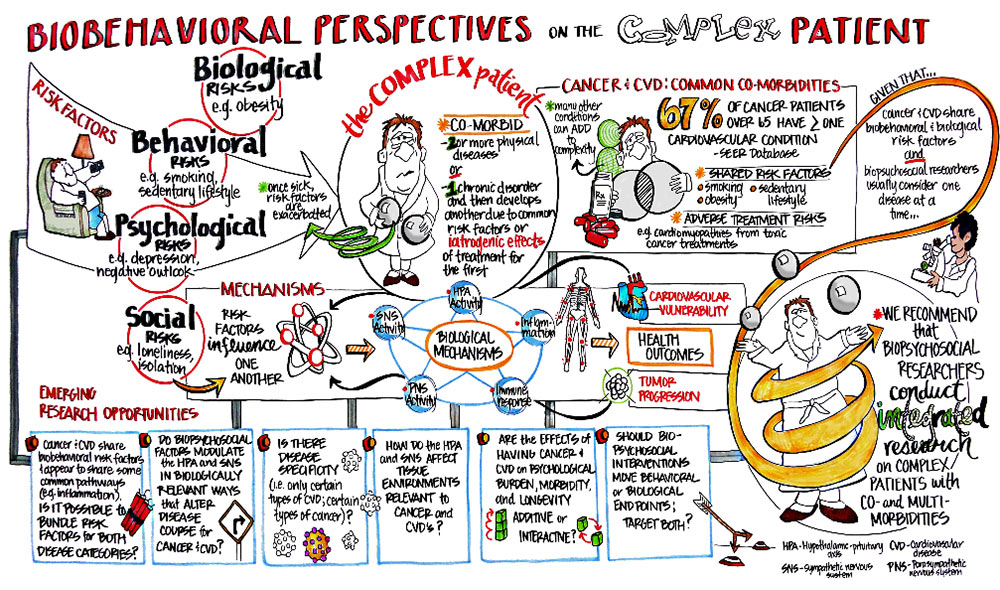
Many risk factors that contribute to disease: biological risks (e.g. obesity), behavioral risks (e.g. smoking, sedentary lifestyle), psychological risks (e.g. depression, negative outlook), and social risks (e.g. loneliness, isolation). Risk factors influence one another and are exacerbated once someone is sick. The biological mechanisms that lead to cardiovascular vulnerability, tumor progression and overall health outcomes are multifactorial. These include Sympathetic Nervous System (SNS) activity, Parasympathetic Nervous System (PNS) activity, the Hypothalamic-Pituitary-Adrenal (HPA) axis, Inflammation and the Immune response.
The "complex patient" has a "co-morbid condition," meaning they have two or more physical diseases or they have one chronic disorder and develops another due to common risk factors or iatrogenic effects of treatment for the first.
The combination of cancer and cardiovascular disease (CVD) is a common co-morbid condition. Sixty-seven percent of cancer patients over 65 have more than one cardiovascular condition (SEER database). The shared risk factors of Cancer and CVD include smoking, obesity and sedentary lifestyle. There are also adverse treatment risks associated with this co-morbidity (e.g. cardiomyopathies from toxic cancer treatments). Many other conditions can add to the complexity of this co-morbidity.
Given that cancer and CVD share biobehavioral & biological risk factors and biopsychosocial researchers typically consider one disease at a time, we recommend that biopsychosocial researchers consider integrated research on complex patients with co- and multi-morbidities.
Biobehavioral perspectives on the complex patient (PDF)
Visual report created by:
Facilitation | Foresight | Strategy
Emerging research questions include:
- What are the shared biobehavioral risk factors and common pathways (e.g. inflammation) among cancer & CVD patients?
- Do biopsychosocial factors modulate the HPA and SNS in biologically relevant ways that alter disease course for cancer and CVD?
- Is there disease specificity (i.e. only certain types of CVD; certain types of cancer)?
- How do the HPA and SNS affect tissue environments relevant to cancer and CVD’s?
- Are the effects of having cancer and CVD on psychological burden, morbidity, and longevity additive or interactive?
- Should biopsychosocial interventions move behavioral or biological endpoints; target both?
Special issue about multimorbidity
This special issue highlights how health psychology and behavioral medicine can contribute to understanding, preventing, and controlling the growing prevalence of multimorbidity.
-
Multimorbidity: Implications and directions for health psychology and behavioral medicine
Jerry Suls, Paige A. Green, and Cynthia M. Boyd
-
The measurement of multimorbidity
Kathryn Nicholson, José Almirall, and Martin Fortin
-
Inflammation in multimorbidity and disability: An integrative review
Elliot Friedman and Carrie Shorey
-
Jeffrey L. Birk, Ian M. Kronish, Nathalie Moise, Louise Falzon, Sunmoo Yoon, and Karina W. Davidson
-
Xiaolin Xu, Gita D. Mishra, and Mark Jones
-
Exercise in people with comorbidity or multimorbidity
Joost Dekker, Bianca M. Buurman, and Marike van der Leeden
-
Multimorbidity in randomized controlled trials of behavioral interventions: A systematic review
Carolyn R. T. Stoll, Sonya Izadi, Susan Fowler, Sydney Philpott-Streiff, Paige Green, Jerry Suls, Anke C. Winter, and Graham A. Colditz
-
Toward a health-promoting system for cancer survivors: Patient and provider multiple behavior change
Bonnie Spring, Tammy Stump, Frank Penedo, Angela Fidler Pfammatter, and June K. Robinson
Suls J, Bayliss EA, Berry J, et al. Measuring Multimorbidity: Selecting the Right Instrument for the Purpose and the Data Source. Med Care. 2021 May 11. doi: 10.1097/MLR.0000000000001566 ![]() .
.
Salive ME, Suls J, Farhat T, Klabunde CN. National Institutes of Health Advancing Multimorbidity Research. Med Care. 2021 Apr 23. doi: 10.1097/MLR.0000000000001565 ![]() .
.

